What is laparoscopy?
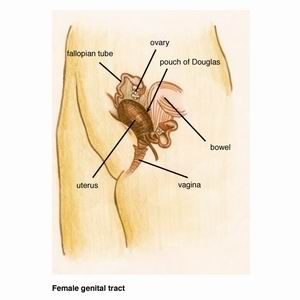
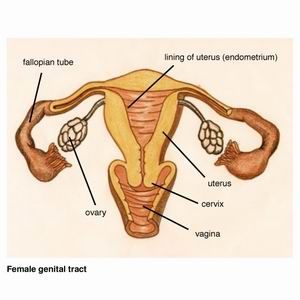
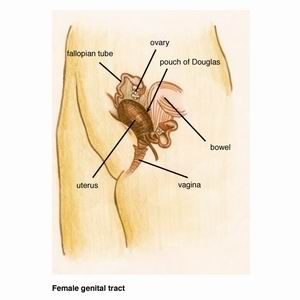
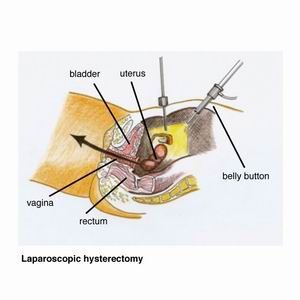
Laparoscopy is an operation which allows the surgeon to see and operate on the organs inside the pelvis and abdomen (belly). The pelvis is the basin-shaped cavity at the lower end of the body formed by the left and right hip bones and includes the genital region.
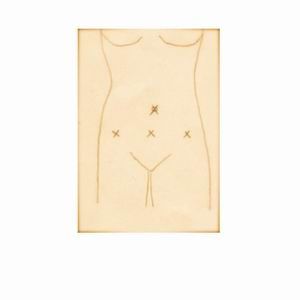
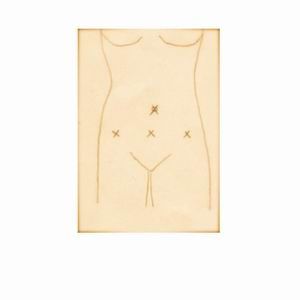
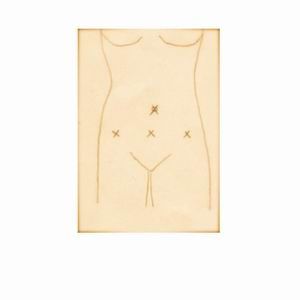
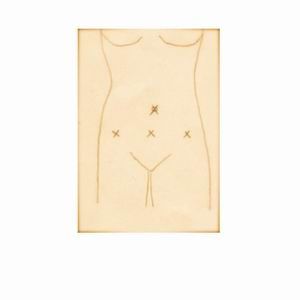
A small 5 to 10 mm incision (cut) is made in the belly button through which the laparoscope (this is like a telescope) is inserted with a video camera attached. Further instruments are inserted through another three little cuts in the lower abdomen.
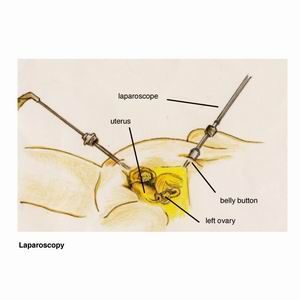
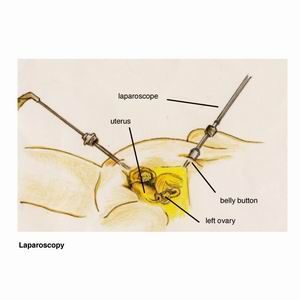
Carbon dioxide gas is used to distend the abdomen. This is inserted through a needle via the belly button, but this may not be possible in all cases. Therefore a larger incision through the belly button may be required or a needle may be placed just below the left ribcage.
At the time of the laparoscopy an instrument (uterine elevator) is inserted via the vagina into the uterus. This allows the surgeon to lift and move the uterus which is required for the laparoscopy.
A video and/or photos will be taken during the operation and used to show you what was seen and done. Dr Varol will send you a copy of the operation report together with the photos taken before and after surgery.
Laparoscopy has many advantages over open surgery, small incisions versus a bigger cut, like we do for a caesarean section, is one of them.
Laparoscopy's advantages over open surgery are:
- less pain
- faster recovery
- quicker return to normal activities
- minimal scarring
- lower risk of infection
A laparoscopy is done under a general anaesthetic, so you are asleep for the operation.
Some of the reasons to perform a laparoscopy are the following:
Endometriosis
The surgeon is able to remove endometriosis and free adhesions. An adhesion refers to tissues or organs that are stuck together, when naturally they should be apart.
Hysterectomy
A hysterectomy (removal of the uterus) can be detached from the surrounding tissue with the instruments that are inserted through the little laparoscopy incisions (cuts) in the tummy. The uterus is then removed through the vagina, thus avoiding the need to make a large incision. This operation usually a three day stay in hospital and most patients return to full activity within three weeks.
Ectopic Pregnancy
An ectopic pregnancy is a pregnancy that occurs outside the uterus, usually in the fallopian tubes. Three incisions are made in the abdomen and the fallopian tube is removed at laparoscopy.
Fibroid
Depending on the size and position of fibroids, they can be removed at laparoscopy without needing to make a larger incision in the abdomen.
Investigation of infertility and pelvic pain
Some of the causes of infertility and pelvic pain can be treated successfully at laparoscopy, such as endometriosis and adhesions.
Diet before your laparoscopy
You will be given a diet form which explains in details what you can and cannot eat before your laparoscopy. This is very important as your bowels need to be empty for the operation. If you have endometriosis or other disease that is near or on the bowel, then this can only be removed if the bowel is empty. If the operation is scheduled for the afternoon at Royal Prince Alfred Hospital, you need to stop eating and drinking at 6 am the morning of your surgery.
Medication
It is important to continue to take your usual medications such as those for high blood pressure, diabetes and the oral contraceptive pill. If you have been taken non steroidal anti-inflammatory medications such as aspirin, Ponstan, Nurufen, Naprogesic etc, you should stop them 14 days before your operation. You may take tablets that contain paracetamol and codeine such as Panadol, Panadeine or Panadeine Forte for pain relief.
Hospital Stay
You will be admitted to The Perioperative Unit at Royal Prince Alfred Hospital for one night if you are having a laparoscopy. This is located on the third floor of the hospital. If you are admitted for a hysterectomy or an open surgery (laparotomy), you will be shown to one of the wards in the hospital and your hospital stay will take a few days.
You will be taken to the operating theaters in a bed and the anaesthetist will see you and explain what is going to happen before you fall asleep. He will put a cannula into one of the veins in your hand or arm. He will give you some medication to make you feel relaxed and you will then be taken into the operating room. The anaesthetist will place a mask on your face for you to take some deep breaths of oxygen. He will then administer anaesthetic drugs through the drip in your arm and you will fall asleep.
When you wake up, you will find yourself in the Recovery Room where there is a nurse who will look after you. You will be given drugs to keep you comfortable and pain free. After half an hour to an hour you will return to your initial ward. Dr Varol will see you after the operation and explain the surgery to you, what was found and what was done. You will also be seen the next morning before you go home.
After Your Operation
You will need someone to look after you for about two to three days when you come home. In general you will need one week off from week. Some women may need two weeks recovery at home.
Wounds
In general you will have 4 small wounds in your tummy which have dressings on them. There will be a little bit of blood underneath the dressings which is normal. They are waterproof and you can take a shower as usual. Take the dressings off 4 days after your operation, i.e. if your operation was on Tuesday at Royal Prince Alfred Hospital, you should take them off on Saturday.
In general there will be a stitch underneath the skin in the belly button wound which will dissolve by itself. The other wounds won't have a stitch but steri strips which are strong sticky tapes for wounds. Sometimes a stitch may need to be placed in those wounds as well and they usually dissolve by themselves. If stitches need to be removed, Dr Varol will inform you after the operation.
Pain
Because the wounds from laparoscopy are very small, they heal fairly quickly with minimal scarring. There will be some pain from the operation and you will be given a script for Panadeine Forte which you will need for a few days. Every day you should feel better than the previous day. If you suddenly feel worse or have more pain, please contact Dr Varol. You can contact her 24 hours a day.
Diet
It is best to have a healthy diet after your operation with fruits, vegetables & lean meats. You should avoid fatty & fried foods. It's easy to become constipated after an operation, so have plenty of fluid to drinks & eat some fruits. Fruits that are particularly good for constipation are prunes and guavas. You may need to take some extra medication such as Metamucil or coloxyl and senna tablets.
If you had part of your bowel removed, your diet will be different and Dr Varol will explain that to you. In general she will want you to be on a fluid diet for a few days before you start on solid foods.
Work
In general you need one week off from work after a laparoscopy. Some women may need two weeks, depending on how you are recovering and your type of work.
Driving
As with any procedure that requires a general anaesthetic, you must not drive for the first 24 hours after discharge from hospital. A responsible adult needs to pick you up from hospital and take you home. If you had a hysterectomy or an open operation, you should not drive for four to six weeks.
Return to Normal Activities
Recovery time depends on the individual and the type of operation you have had. In general you will find it too uncomfortable to do any kind of heavy work or exercise such as vacuuming, carrying heavy things, aerobics etc for a few weeks. The general rule is that if an activity makes you feel tired or gives you pain or discomfort, you should not do it. Dr Varol will let you know how long it will take you to get back to normal activity.
Sex
After a laparoscopy you may resume sexual activity when you feel comfortable enough and there is no more bleeding from the vagina. That usually takes one to two weeks. If you had a hysterectomy, the stitches in the top of the vagina need to heal before you can have sex again. That takes about four to six weeks.
Complications of laparoscopic surgery
Please see the section under ?Consent for Laparoscopic Surgery? for the details of the possible complications with laparoscopic surgery.
Follow up appointment
In general you should ring Dr Varol's practice to make an appointment for four weeks after your operation. If you have any problems, concerns or questions, please ring her as per details below.
Dr Varol's contacts details
office hours :
Ring her practice on 9223 7200
after hours :
Ring Royal Prince Alfred Hospital (RPAH) on 9515 6111 and ask switchboard to page Dr Varol. Leave your name and number and Dr Varol will call you back promptly. If there is a problem, ask switchboard to put you through to her mobile number.
What is hysteroscopy?
Hysteroscopy is a procedure where an instrument called a hysteroscope (this is like a telescope) is inserted into the uterus (womb) so the surgeon can see the inside walls and shape of the uterus.
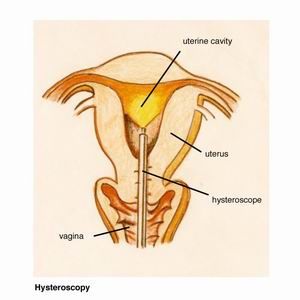
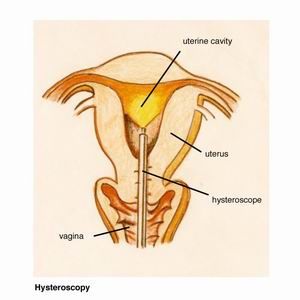
The hysteroscope is inserted through the vagina, cervix and into the uterus. No incisions are necessary.
This procedure may be done for the following problems :
- heavy or abnormal periods
- bleeding after menopause
- ultrasound suggests there is a polyp (non-cancerous tumour of the lining of the uterus) or fibroid (non-cancerous tumour composed of fibrous tissue) inside the uterus
Hysteroscopy only takes a few minutes and is done as a day procedure.
What happens at hysteroscopy?
The anaesthetist will insert a cannula into your hand or arm through which he will give you some drugs to sedate you. The anaesthetic for a hysteroscopy is light and not a general anaesthetic. You will not be asleep but feel quite sedated. There will be no pain and you will not be aware of the procedure. An antibiotic will be given at the beginning of the procedure.
Your legs will be placed in stirrups and a speculum inserted into the vagina. A speculum is the instrument we use to take a Pap smear. It holds the vaginal walls open and allows the surgeon to see the cervix which is the opening of the uterus. Dr Varol will then give further local anaesthetic around the cervix to help with pain relief after the operation.
A hysteroscope is then gently passed from between the legs, through the vagina and cervix into the uterus. Fluid is instilled into the uterus to open up its wall so the lining can be seen well. If there is something inside the uterus such as a polyp or fibroid, the cervix needs to be opened up further so that the polyp or fibroid can be cut out. If all looks ok, a curettage is done. This means an instrument is passed into the uterus and biopsies are taken (pieces of the lining are taken).
How will I feel after a hysteroscopy?
Because the anaesthetic given is very light, most women wake up quite well and can go home after an hour or two. Some women may feel a little woozier than others. There may be slight tummy discomfort or cramping (like period cramps) for which we can give you pain relief.
You will have light bleeding for a few days after a hysteroscopy. Sometimes it can last for up to two weeks. It should not be more than the flow of a normal period.
Complications of hysteroscopy
The risks for a diagnostic hysteroscopy, where the surgeon just needs to see the lining of the uterus and take biopsies, is small. Specific risks include :
- perforation (making a hole) of the uterus with the hysteroscope or other instruments Although uncommon, this risk is slightly higher in postmenopausal women or those who have recently had a baby. A perforation usually heals fairly quickly by itself but, rarely, further surgery may be needed.
- damage to organs nearby If perforation occurred, damage to bowel, blood vessels or bladder can result. This may require further surgery by a laparoscopy or rarely a laparotomy (open surgery).
- infection This is uncommon at hysteroscopy. If a bad smelling vaginal discharge and tummy pain occur, antibiotics will be necessary to clear the infection.
- bleeding
- fluid absorption
When a fibroid is cut out, fluid is required to distend the uterine cavity. Some of the fluid can be absorbed in the body and an imbalance can occur in the blood. This would require further observation in hospital and special fluid through the drip.
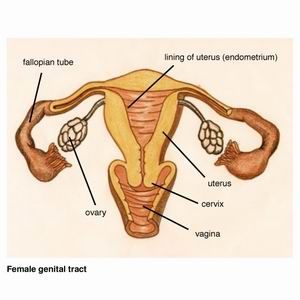
Hysterectomy is the surgical removal of the uterus. The uterus is the organ where pregnancy occurs and a baby grows. Also the uterus is responsible for monthly periods. The lining of the uterus comes away and bleeding happens every month.
What changes happen after a hysterectomy?
After the uterus is removed :
- no more periods occur
- a woman cannot become pregnant and have any more children
- menopause (?change of life?) may occur a year or so earlier than if a hysterectomy had not been done
The uterus does not produce any hormones, it is the ovaries that do. So the hormones in the blood will not change. Your doctor will discuss with you before the operation to decide whether the ovaries are going to be removed or not. If the ovaries are removed, then menopause will occur after the operation as the hormone levels decrease very quickly.
Why do I need a hysterectomy?
Some of the reasons for a hysterectomy are the following :
Heavy or irregular menstrual bleeding
where conservative approaches have been unsuccessful.
where conservative approaches have been unsuccessful.
Prolapse of the uterus
This is a condition where the uterus protrudes into the vagina. In the more severe cases, the uterus can come outside the vagina between the legs. If a woman is not sexually active, she may choose the conservative approach of having a ring put into the vagina to keep the uterus in place. Otherwise a hysterectomy can be performed or a laparoscopy done and the uterus pulled upwards with a synthetic mesh material which is then attached to the upper part of the tailbone (sacrum).
Endometriosis & Adenomyosis
In endometriosis the uterus is normal and removal of the uterus and / or ovaries would only be needed in the most severe cases or where endometriosis has recurred persistently despite surgery by an endometriosis expert and other hormonal treatments. Adenomyosis occurs when the lining of the uterus grows into the muscle. This is a common cause of period pain and heavy periods.
Cancer of the uterus, ovaries or cervix
What types of hysterectomies are there?
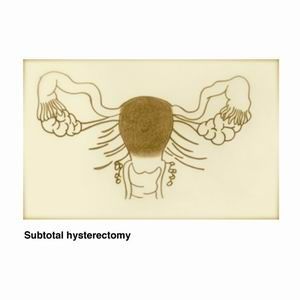
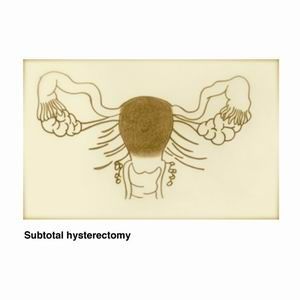
There are 2 types of hysterectomies for benign (non cancerous) problems :
A total hysterectomy involves removal of the entire uterus, including the cervix. The ovaries may be kept or removed.
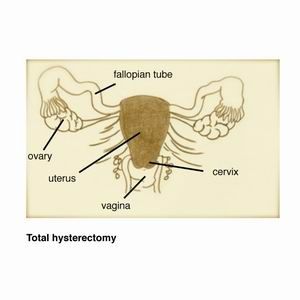
Subtotal hysterectomy is the removal of the upper part of the uterus. The cervix is kept. The advantage of this operation is that the cervix continues to support the top part of the vagina and prolapse of the vagina after a hysterectomy is less common. Some studies also report that sexual function might be better. However then there are equally other studies to suggest that taking the cervix makes no difference to sexual function. The ovaries may be kept or removed.
How is a hysterectomy done?
There are three ways in which the uterus can be removed. Your doctor will discuss these with you and the decision for a particular one is based on the doctor"s surgical experience, the size and shape of the uterus and whether there is prolapse of the uterus into the vagina.
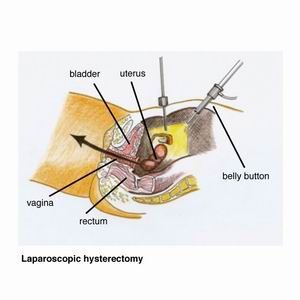
1. Laparoscopic hysterectomy
A laparoscopy is an operation where a telescope-like instrument is inserted through a 1 cm cut in the belly button. Three other small cuts are made lower in the tummy. The uterus is then detached from its structures in the pelvis and removed through the vagina. This is also called ?key hole surgery?. Please read the section under ?laparoscopy? for further information.
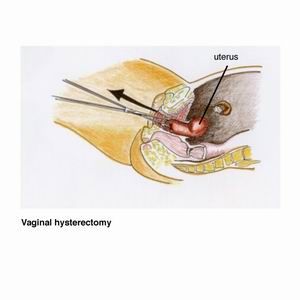
2. Vaginal hysterectomy
If there is some prolapse of the uterus, the uterus can be removed through the vagina without any cuts in the tummy. Prolapse means that the uterus has moved downwards into the vagina to some degree. This happens particularly to women who have had many babies delivered vaginally.
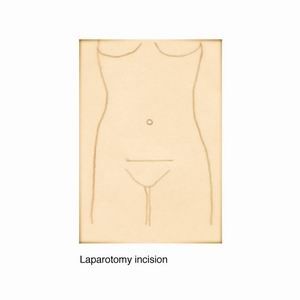
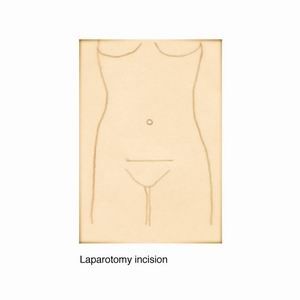
3. Abdominal hysterectomy
An incision (cut) is made in the tummy like the one we do for a caesarean section to deliver a baby. This is also called an open operation or laparotomy. An abdominal hysterectomy would be the operation of choice if the uterus is very large, there are other extensive problems in the tummy such as severe endometriosis or adhesions from previous infection or operations. If the surgeon believes a hysterectomy will take a long time due to lots of problems in the tummy, then an abdominal hysterectomy might be the operation of choice.
Are there alternatives to a hysterectomy?
These days the decision for a hysterectomy is not made lightly. Hysterectomy is usually the last resort to a problem that has not responded to conservative management. However a woman may equally choose a hysterectomy as one of the earlier options of her treatment after discussion with her doctor.
If a woman has heavy periods, for example, she may choose one of the many conservative options. There are medical and surgical treatment options which are outlined in the section ?heavy menstrual bleeding?.
What are possible complications of a hysterectomy?
Every operation and treatment has potential side effects. A hysterectomy has risks associated with it despite the highest standard of surgical practice. It is a matter of a woman weighing up the risks against the benefit she will get from a hysterectomy. A hysterectomy is performed under general anaesthetic, so you will be asleep. Modern anesthesia is safe and effective, but does have risks. Rarely side effects from an anaesthetic can be life threatening.
Dr Varol will explain the major and most important potential risks to you and give you a pamphlet from the Royal Australian & New Zealand College of Obstetricians & Gynaecologists on hysterectomy for your reading. You can then write down questions you have and discuss them with her at the next consultation. Have as many consultations as you feel you need to be able to make a decision for or against a hysterectomy. An operation should never be done until you are happy that you understand everything, you feel all your questions have been satisfactorily answered, and are psychologically ready for it. All the alternatives to a hysterectomy should be explained to you and the advantages and disadvantages of all treatments discussed. The decision to have surgery is always yours and should not be made in a rush.
General risks of hysterectomy
- infection of the wounds, bladder, chest, bloodstream, or inside the tummy
- bleeding
- keloid scar -Sometimes an incision heals by scarring and the wound will look raised and thicker than normal. It is more common in women who have darker skin.
- cardiovascular problems - This refers to heart attacks, blood clots or stroke which depends on the medical history of the women.
Specific risks of hysterectomy
- haemorrhage - A large blood loss would require blood transfusion.
- injury to organs which are around the uterus, such as bowel, bladder, ureter (tube that connects the kidneys to the bladder), and blood vessels
- Rarely during laparoscopy a bubble of the gas used for laparoscopy, carbon dioxide, may get into the blood stream and travel to the heart. This is called a ?gas embolism? and, although rare, can cause death.
- Persistent Pain. Discuss with your doctor what the possible outcome will be for you from the hysterectomy. If the hysterectomy is done for chronic pain, the pain may continue after the uterus is removed.
Further surgery may be required to treat a complication that has occurred.
How will I recover after a hysterectomy?
For laparoscopic & vaginal hysterectomy :
hospital stay is about 2 days
hospital stay is about 2 days
recovery at home is about 1-3 weeks
For abdominal hysterectomy :
hospital stay is about 3-5 days
recovery at home is about 4-6 weeks
Pain relief
You will some pain in your tummy after a hysterectomy and your doctor will give you painkillers to take at home. Take them regularly in the early days you are at home and then you can gradually reduce them and only take them when you need them. Painkillers can make you constipated, so make sure you drink plenty of water and eat fruit.
After a laparoscopy it is normal to feel some pain or discomfort in the shoulders and chest. This is from the gas carbon dioxide that is used for the operation. The gas gets released from the tummy at the end of the operation but some stays inside. It takes 24-48 hours for this discomfort to go away.
Diet
There may be some nausea and constipation after a hysterectomy which will settle. It is a good idea to have small and frequent meals after a hysterectomy, rather than 3 big meals. The food should not be heavy or fried but easy to digest.
Mobilization
In hospital you would have been wearing TED stockings which help to prevent deep vein thrombosis of the legs. Continue to wear them at home until you are fully mobile as before the operation. You can take the stockings off for washing. It is good to do some walking every day, depending on how comfortable you are. Do not lift heavy things or do vigorous exercise for about 4 - 6 weeks.
How will I feel after a hysterectomy?
Sadness
Whilst a woman may feel very pleased to have had a hysterectomy because her problems have disappeared, she may at the same time feel sad or depressed about the loss of her uterus. Even though a woman has completed her family or did not wish to have children and was very certain that a hysterectomy was the correct option for her, she may still have these emotions. It is important to consider how a hysterectomy may make you feel and discuss this with your doctor, a friend or family member.
Sex
It is usually advised not to have vaginal intercourse for about 6 weeks after a hysterectomy because it takes that long for the top of the vagina to heal.
Menopause
If the ovaries have been removed together with the uterus, a woman may have symptoms of the menopause such as hot flushes, dry vagina, difficulty sleeping etc. Depending on how much the symptoms affect a woman"s life, she may choose to take hormone replacement therapy. Other important advice is to take calcium tablets and do regular weight bearing exercises to protect the bones from osteoporosis (bone loss).
Do I need to continue with Pap smears after a hysterectomy?
If you had normal and regular Pap smears prior to the hysterectomy and the hysterectomy was done for a benign (non cancerous) problem, then no further Pap smears are needed.
If you had abnormal Pap smears prior to the hysterectomy, then you must continue with Pap smears. The Pap smear is then taken from the top of the vagina to make sure that the abnormality which was present in the cervix of the uterus does not come back in the vagina.
Downloadble Information Packs
Click on the heading below to download and view the information in PDF format.
Laparoscopy consent form [Adobe Acrobat PDF - 407.4 KB]
Diet before surgery form [Adobe Acrobat PDF - 281.1 KB]
Instructions after laparoscopy form [Adobe Acrobat PDF - 469.72 KB]
Instructions after hysteroscopy form [Adobe Acrobat PDF - 370.13 KB]
Instructions after LEEP form [Adobe Acrobat PDF - 414.31 KB]