Your Health
This information package is designed for general information and is not a substitute for a medical opinion. It will help you to make an informed decision after you have discussed your options with your doctor and a tailor-made care plan has been formulated.
ENDOMETRIOSIS
What is endometriosis?
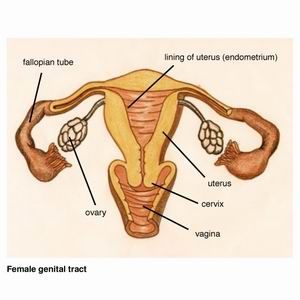
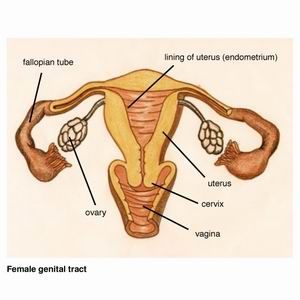
The uterus (womb) has a cavity in which a baby grows. Part of this lining (called endometrium) is shed every month and results in menstruation (a period). When this lining grows outside the uterus, we call it endometriosis. One in ten women (10%) of menstruating age have endometriosis, so it is considered common. It can occur from the age of puberty until the menopause.
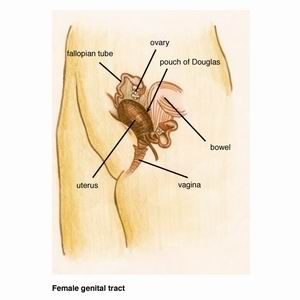
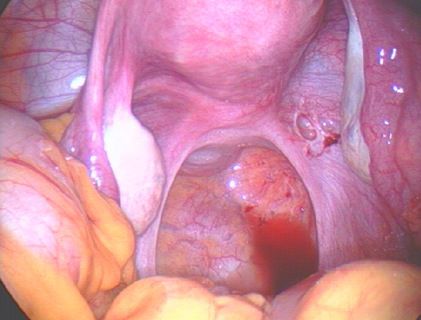
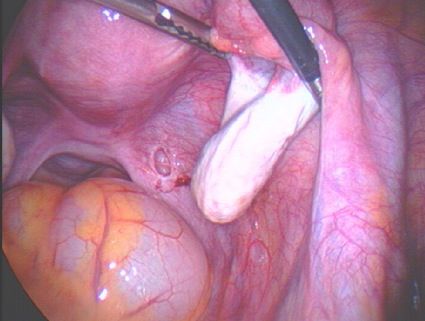
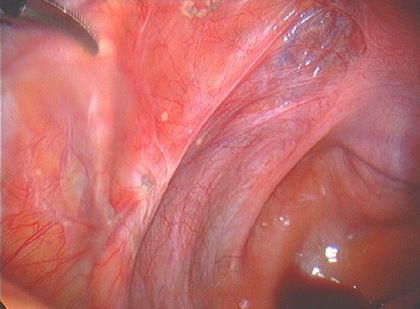
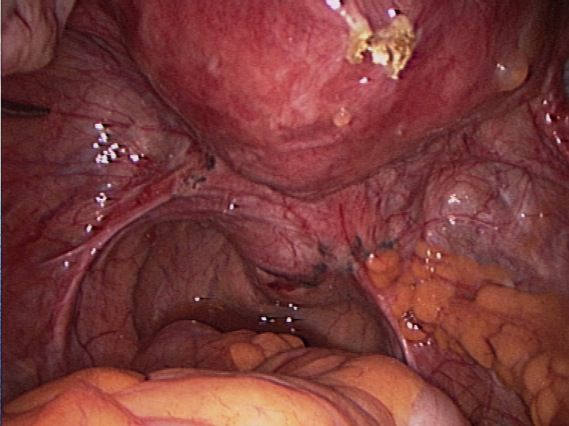
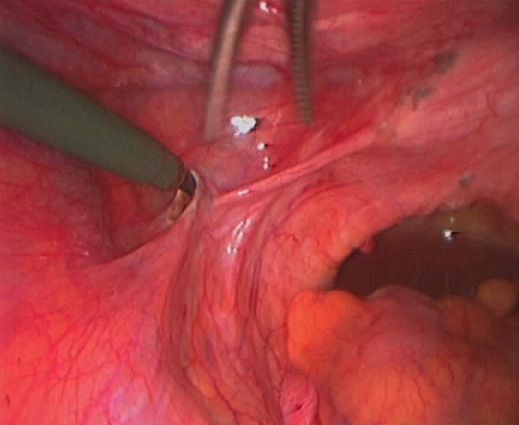
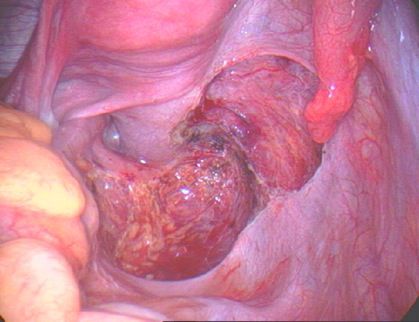
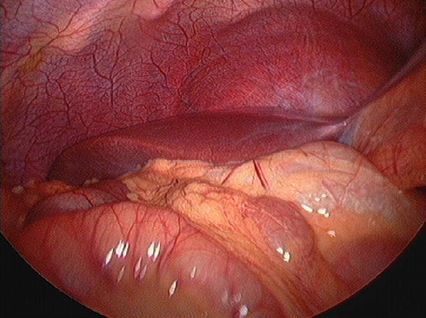
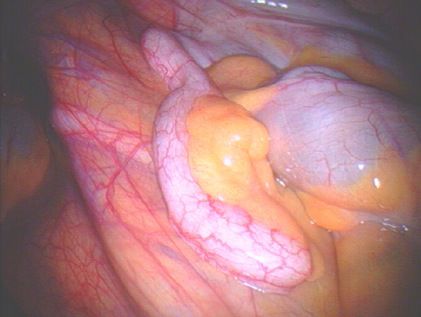
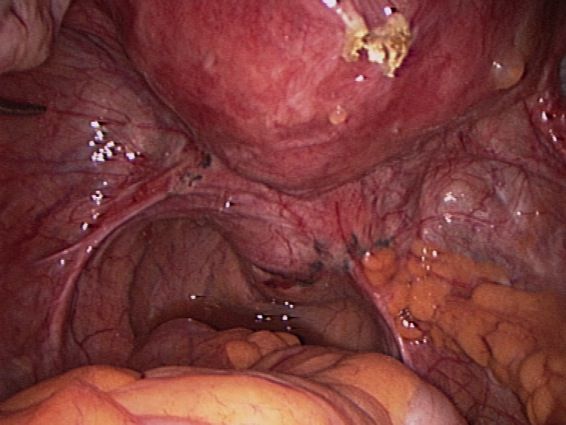
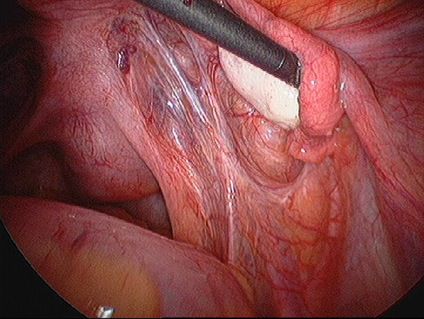
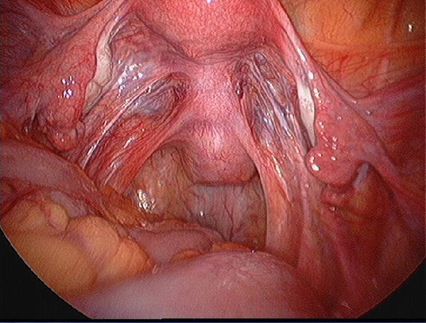
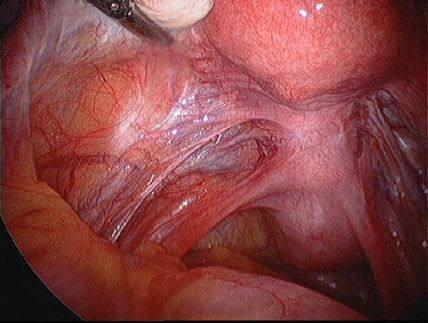
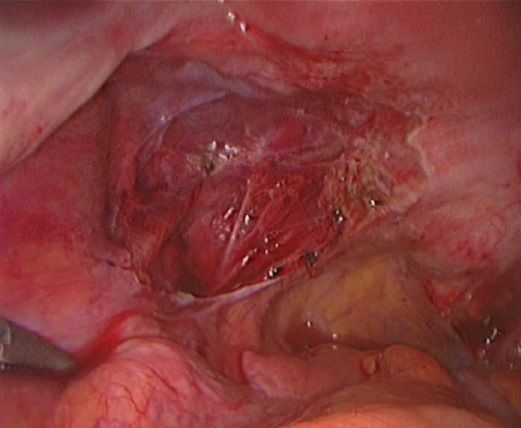
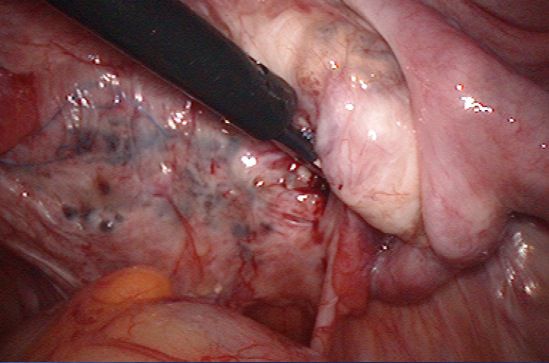
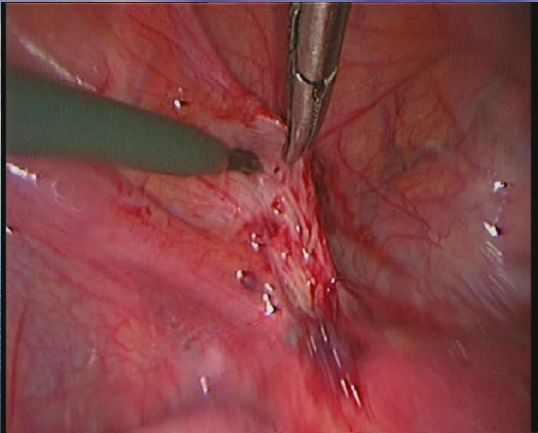
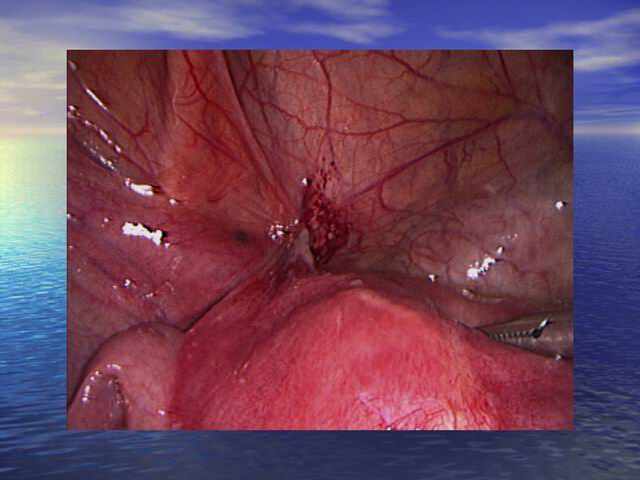
Endometriosis causes scar tissue and can result in the uterus, ovaries, fallopian tubes and bowel becoming stuck to each other and to the lining of the tummy. Here are some photos of what endometriosis looks like and photos of endometriosis that has been excised (cut out) for treatment.
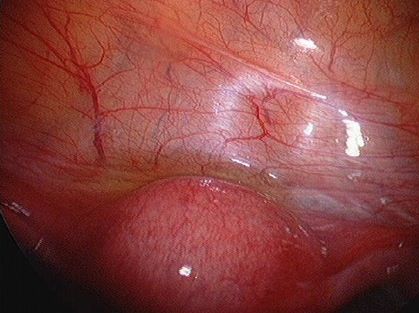
| Normal pelvis with normal uterus, ovaries, fallopian tubes and Pouch of Douglas. |
| Endometriosis of lining of right pelvic sidewall & uterosacral ligament. |
| Endometriosis of lining of right pelvic side wall & uterosacral ligament. |
| Endometriosis of lining of left pelvic sidewall. |
| Endometriosis of both pelvic sidewalls, uterosacral ligaments & Pouch of Douglas. |
| Endometriosis on lining of left pelvic sidewall and in Pouch of Douglas. |
What causes endometriosis?
Although the exact cause of endometriosis is still unknown, there are a number of theories about how it develops. It is believed that a number of causes exist together to cause this disease.
The most likely explanation is that cells lining the tummy change into the type of cell that line the uterus. Some endometriosis probably results from menstrual fluid flowing backwards through the fallopian tubes and deposits in the tummy. There is a genetic component to endometriosis and women who have a mother or sister with endometriosis, are more likely to have it as well. There is a change in the immune system in women with endometriosis. Most women have a natural defense which gets rid of menstrual fluid in the tummy. Women with endometriosis have a reduced ability to clear it or to prevent its growth once it has settled on the lining of the tummy. The hormone oestrogen produced by the ovaries is also required to grow endometriosis. That is why after the menopause when the ovaries stop functioning and the oestrogen becomes very low, usually the pain with endometriosis settles down.
Factors reducing the risk of endometriosis
1. Aerobic exercise of five hours per week has been shown to reduce the risk of recurrence of endometriosis.
2. Having a child reduces the risk of recurrence by about 50%.
3. Similar to pregnancy, the oral contraceptive pill also has a protective effect. It keeps the ovaries quiet and there is no ovulation (egg production and release). The pill prevents the surge in oestrogen that normally occurs.
What problems does endometriosis cause?
Pain with periods
This is the most common pain with endometriosis. Period pain usually starts with the first time a woman has her periods. In many women period pain may start after many years of having fairly pain-free periods. These women particularly are likely to have endometriosis. However one needs to remember that about 70% of women in the world have period pain that is normal without any underlying reason except that they are having periods. A woman may not have any pain despite quite advanced endometriosis. She may see her doctor because she cannot get pregnant. The severity of endometriosis often does not correlate with the severity of pain. Women with little endometriosis may have a lot of pain or they may have a great deal of endometriosis and not much pain at all.
Pain with sex
If there is endometriosis on the vagina and forms scar tissue, it can be painful during sex because the vagina cannot stretch. Pain may also occur due to nerves being involved in that area. Pain can particularly be painful when vaginal intercourse occurs just prior to periods (or during periods if vaginal intercourse occurs during that time).
| Endometriosis has been cut out from the back of the vagina |
Pain when opening bowels
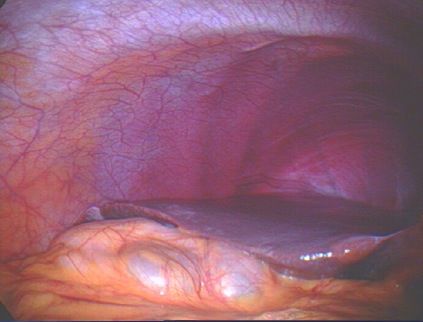
Pain that occurs when a woman opens her bowels is usually an indication of advanced endometriosis. Endometriosis would involve the wall of the bowel or may just cover the space between the uterus, vagina and bowel. This area is called the pouch of Douglas and basically is the area a woman sits on, that is, the bottom of the tummy. Here is a diagram and a photo of this area.
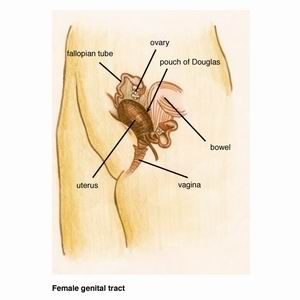
| Normal back wall of vagina, pouch of Douglas & uterosacral ligaments |
| Severe endometriosis with distortion of pelvic anatomy. Endometriosis on back of uterus. Rectum (lower part of bowel) is attached to vagina and uterus. Left ovary attached to back of uterus. |
Pain when opening bowels can sometimes be so severe that a woman is doubled over in pain on the bathroom floor.
Examination
A gynaecological examination by your doctor is very important. Your GP or gynaecologist would have a feel of your tummy, and then examine the vagina with a speculum. This is the instrument used to take a Pap smear. A vaginal examination is then performed which may reveal an area of tenderness. The doctor may also feel some nodularity in the vagina which would indicate scar tissue behind the vagina or on the bowel.
Often the gynaecological examination is perfectly normal. This does not exclude endometriosis, as a woman may still have mild or moderate disease which has not caused significant scar tissue to be able to be felt on vaginal examination.
Ultrasound
The only abnormality an ultrasound would pick up is a cyst of endometriosis in the ovaries. This is called a ?chocolate cyst? because it is filled with old blood that looks like melted chocolate. When we see chocolate cysts in the ovaries, it usually means advanced endometriosis. In general these cysts develop once endometriosis has grown in a lot of areas of the tummy already.
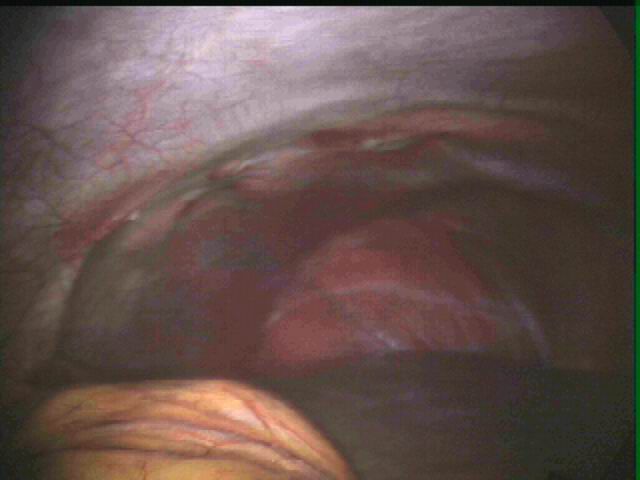
Laparoscopy
Laparoscopy is the only way we can make a definite diagnosis of endometriosis. This is also called ?keyhole surgery? which is done under general anaesthetic in hospital. Very small cuts (half a centimeter) are made in the tummy and a laparoscope (this is like a telescope) is inserted through the belly button. The laparoscope is connected to a camera and television, so the surgeon can visualize all the gynaecological organs.
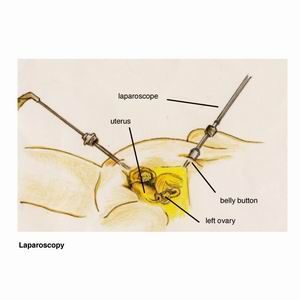
Here are photos of what a normal pelvis and abdomen look like.
| Normal pelvis with normal uterus, ovaries & fallopian tubes |
| Normal liver and diaphragm |
| Normal appendix |
| This is the area in front of the uterus where the bladder is. The lining between the uterus & bladder is normal in this photo. |
If endometriosis is present, the surgeon excises it (cuts it out). Laparoscopic excision of endometriosis requires a high degree of skill by the surgeon. Therefore the surgeon would have had special training in this type of operation.
Laparoscopy has many advantages over open surgery where a big cut is made in the tummy, like a caesarean section cut. Women experience much less pain, recover more quickly, there is minimal scarring and reduced risk of infection
Please have a look under the heading "Laparoscopy"
Peritoneum
The peritoneum is the lining of the pelvic organs. Endometriosis most commonly affects the peritoneum.
| Endometriosis of both pelvic sidewalls, uterosacral ligaments & Pouch of Douglas |
| Superficial endometriosis of right pelvic sidewall peritoneum |
| Superficial endometriosis of both pelvic sidewall peritoneum |
| Superficial endometriosis of left pelvic sidewall peritoneum |
| Endometriosis of both uterosacral ligaments |
| Excised (cut out) endometriosis of left uterosacral ligament |
| |
Ovary
A cyst of endometriosis in the ovary is called a ?chocolate cyst? because it is filled with old blood that looks like melted chocolate. The medical word for it is endometrioma. Here is an example of an endometrioma.
| Endometriosis of right pelvic sidewall extending underneath ovary. Right ovary densely attached to sidewall. |
Uterus
Endometriosis is often seen on the back of the uterus where it affects the outer layer. One can see reddish or clear coloured areas of endometriosis.
Here is an example of endometriosis affecting the uterus.
| Severe endometriosis with bowel attached to uterus. Only top of uterus can be seen. |
Rectum and vagina
When endometriosis affects the vagina, women often feel pain during sex. This occurs because scar tissue prevents the vagina from stretching or because nerves are affected by endometriosis. The rectum is the lowest part of the bowel behind the anus. The anus is where one opens the bowels. When endometriosis affects the bowel, women have pain with sex and on opening bowels. Rarely bleeding from the anus may occur during periods. Here is an example of endometriosis affecting the rectum and vagina.
| Severe endometriosis of vagina and pouch of Douglas. Both ovaries are adherent to pelvic sidewalls. |
| Severe endometriosis. Complete obliteration (blockage) of Pouch of Douglas. The bowel is densely adherent to uterus, so the normal space between vagina & rectum (lower part of bowel) is not present. |
Bladder
Endometriosis often affects the lining over the bladder. Rarely it can go deeper into the muscle of the bladder and cause pain when a women passes urine or there may be blood in the urine. Here is an example of endometriosis affecting the lining over the bladder.
| This is the area in front of the uterus where the bladder is. The lining(peritoneum) between the uterus & bladder is normal in this |
| Endometriosis near peritoneum between uterus & bladder |
| Endometriosis of peritoneum between uterus & bladder |
| Excised endometriosis of peritoneum between uterus & bladder |
Below ribcage or diaphragm
Rarely a women may have endometriosis in the lining underneath the ribs higher up in the tummy. This can cause pain in the upper tummy during periods. Here is an example of endometriosis below the ribcage on the right.
| Normal liver & diaphragm |
| Endometriosis of peritoneum underneath right ribcage |
| Excised endometriosis of peritoneum underneath right ribcage |
Endometriosis and infertility!
Endometriosis is commonly associated with infertility. About 30% of women requiring IVF infertility treatment (in vitro fertilization or ?test tube babies?) have endometriosis. It is important to find out about endometriosis early , so it can be treated and infertility is
prevented or minimized.
Here are some of the previous photos which explain why a woman would not be able to become pregnant. When the anatomy is distorted, the tubes become blocked, the egg does not get picked up by the tube and cannot travel through the tube to implant inside the uterus.
| Severe endometriosis. Complete obliteration of pouch of Douglas. The bowel is densely adherent to uterus, so only top of uterus is visible. No normal anatomy of pouch of Douglas is present. |
| Severe endometriosis of vagina and pouch of Douglas. Both ovaries are adherent to pelvic side walls. |
Other diseases may be confused with endometriosis
Many women have irritable bowel disease with pain in the tummy, bloating, constipation and diarrhoea. The pain may be similar to endometriosis pain. Whilst pain gets better in the majority of women after endometriosis surgery, sometimes scar tissue may form in the tummy which can cause pain that can be similar to the pain of endometriosis.
What endometriosis is NOT associated with
Endometriosis does not cause heavy or irregular periods. If a woman has lots of bleeding with her periods, the doctor will help her with that separately. The only menstrual irregularity endometriosis can cause is some spot bleeding a few days before the proper periods start.
What about drug treatment?
The best drugs for period pain are tablets which are called non steroidal anti inflammatory drugs. These are like aspirin such as Ponstan, Nurufen, Naprogesic etc. They give better relief from period pain than paracetamol (Panadol).
Because not all period pain is from endometriosis, some women decide to try the oral contraceptive pill. The pill acts by preventing ovulation (release of egg from the ovary) and stopping the large oestrogen surge from the ovary. The pill is usually given continuously by skipping the sugar tablets, so that there are no periods. This often causes breakthrough bleeding where bleeding occurs at any time when the pill is taken. So realistically a woman needs to have a proper period on the pill every 3 to 4 months to stop that annoying bleeding.
A woman may decide to take the pill for pain control rather than opt for a laparoscopy because a laparoscopy is an operation with associated risks and she does not want to go down that path.
Studies have shown that after laparoscopic surgery for endometriosis, the disease may come back in about 30% of women. To minimize the recurrence of endometriosis, it is advised to commence hormonal treatment after surgery. The Mirena intrauterine device is often the best way to do that. It is highly effective in reducing the bleeding from periods or may even stop monthly periods and has very little side effects. Alternatively the pill may be given. For women who had severe endometriosis at surgery, she may be treated with a stronger drug called Zoladex for six months before switching to the pill or continuing with the Mirena.
Back to Top
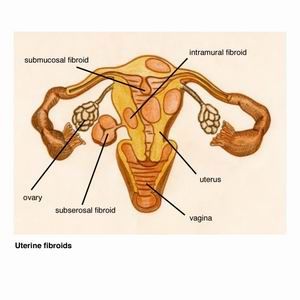
FIBROIDS
What are fibroids?
Fibroids are the most common benign (non-cancerous) growth of muscle and fibrous tissue that grow in the uterus and form a hard ball shaped mass.
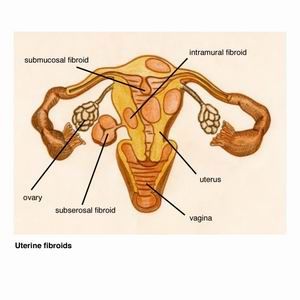
Fibroids that grow inside the cavity of the uterus usually cause the most problems with heavy bleeding. Fortunately they are also the easiest to remove. Fibroids that are on the outside of the uterus, on the other hand, rarely cause a problem.
Fibroids shrink after the menopause when the ovaries stop producing the hormone oestrogen. Fibroids are more common in obese and African women.
The possibility of cancer in a fibroid is very small. This occurs in only about 7 out of 1000 fibroids. This increases as a woman gets older and the risk doubles if a woman is postmenopausal. The small risk of cancer does not justify surgery or a hysterectomy for all women with fibroids. However, unexplained rapid enlargement of a fibroid, particularly in a postmenopausal woman, raises the possibility of cancer and surgery is needed.
What problems do fibroids cause?
There are three main problems fibroids can cause :
1. abnormal vaginal bleeding
Fibroids, especially those that are inside the cavity, can cause heavy periods or bleeding outside periods.
2. pressure on bladder or bowel
If a fibroid is large, it can press on the bladder and cause urgency to pass urine or discomfort when voiding. Pressure on the bowel can rarely cause constipation. A fibroid can also press on the ureter (tube that connects the kidney to the bladder) and cause obstruction to the kidney.
3. infertility & miscarriage
Large fibroids inside the uterine cavity can interfere with getting pregnant or result in miscarriage.
4. pain
Fibroids are usually painless. Rarely when the blood going the fibroid is not enough for its size and growth, the centre of the fibroid goes soft which then can cause pain.
5. abdominal mass
A fibroid may become so big to cause a large swelling in the tummy and a woman may look pregnant.
Do all fibroids need to be removed?
Most fibroids do not cause any problems to a woman and hence can be left alone. Your doctor will probably monitor growth of the fibroid(s) with a physical examination by your doctor and an ultrasound at a specified time, usually in 6-12 months.
If a fibroid causes any of the above problems, treatment would be required.
Treatment
Treatment of fibroids depends on whether the fibroids are causing any problems and whether a woman wants to have children or not. If childbearing is important, then a conservative approach is taken. The options are the following :
Conservative management
Fibroids are not removed and a physical examination and / or ultrasound are done in 6-12 months to check for growth. It is important to note that fibroid surgery in itself can in some cases cause infertility because adhesions occur in the tummy and the tubes can become blocked.
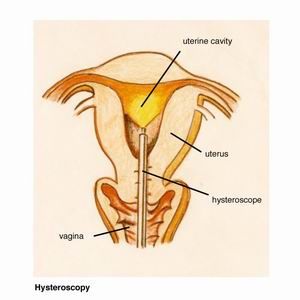
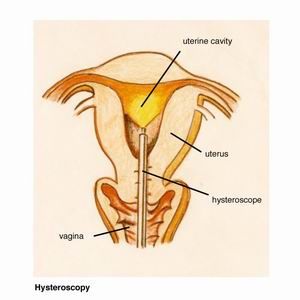
Hysteroscopic resection
If the fibroid is inside the uterine cavity (submucosal), it can be removed by hysteroscopy as a day procedure. Please see section under ?hysteroscopy? for further information. This involves inserting a telescope-like instrument from between the legs into
the vagina and uterus. The fibroid is then cut out.
Myomectomy
This means the fibroid is cut out of the uterus and the uterus is left intact. This is done laparoscopically or with an open procedure, depending on the size and position of the fibroid(s). This would usually mean that deliveries of children would need to be done by caesarean sections. The reason is that a scar would form in the uterus where a cut was made to remove the fibroid(s) and there is a small risk of this scar opening up if the uterus was allowed to contract with normal labour pains.
Because cuts are made into the uterus, some bleeding occurs during the operation. A blood transfusion may be required and there is a small risk of needing a hysterectomy during a myomectomy to stop heavy bleeding.
Uterine artery embolization
This is a day procedure which is performed by interventional radiologists. They are doctors who specialize in ultrasounds, X-rays, CTs, MRI scans etc. Local anaesthetic is given in the groin and a very small cut is made in the skin. A catheter (small tube) is then inserted into the femoral artery and fed upwards until the uterine artery is reached. The uterine artery is the blood vessel that gives blood to the uterus. The uterine arteries are then blocked off by putting a material in it. The fibroid(s) then also will not get any further blood and shrink. It is usually painful afterwards and women need admission to the ward for pain management.
Uterine artery embolization is associated with a 4% risk of ovarian failure. That means that in 4 out of 100 women who have this procedure done, the ovaries will stop functioning and early menopause will happen. Therefore this option is really only for women who have completed childbearing and are in their late forties and older.
Hysterectomy
Hysterectomy means removal of the uterus. That means a woman will not have periods anymore and she will not be able to have any more children. Hysterectomy is therefore reserved for those women who have completed their family and despite more conservative treatments, continue to have problems from the fibroids. Hysterectomy is a good option if fibroids are large and / or involve the cervix. The cervix is the opening part of the uterus which is at the top of the vagina. When a fibroid involves the cervix, it may not be possible to remove the fibroid and leave the uterus because of its position.
Fibroids & Pregnancy
It is not uncommon to be pregnant and have fibroids in the uterus because fibroids are so common. About 20% of fibroids enlarge during pregnancy, 20% decrease in size, and 60% remain unchanged.
Fibroids will never squash or deform a baby inside the uterus. Most pregnancies in the presence of fibroid will proceed without any problems.
Some of the problems a fibroid can cause with pregnancy and delivery are :
Pain
If a fibroid outgrows its blood supply, a part of the fibroid dies and becomes soft. This can cause pain which is treated with non steroidal anti-inflammatory tablets such as Nurufen, Naprogesic, Brufen etc.
Breech or transverse lie of baby
If the fibroid is large enough and in the lower part of the uterus, the baby may not be lying head first but with its bottom first or lie sideways because they are better fits for the baby in the uterus.
Need for caesarean section
Again if the fibroid is large enough and in the lower part of the uterus, the cervix may not open up normally during labour and the baby would need to be delivered by a caesarean section.
Bleeding after delivery of baby
Fibroids may prevent the uterus to shrink after delivery of the baby, and bleeding can result. This may require a blood transfusion and further intervention to stop the bleeding.
Back to Top
HEAVY MENSTRUAL BLEEDING
A woman"s menstrual flow is considered heavy if one or more of the following is present:
1. Increase in the number of times pads or tampons that have to be changed (usually more frequent than every four hours or more than once at night)
2. Bleeding that lasts more than seven days
3. Clots larger than three centimeters
4. Flooding (accidents where blood goes through a tampon or pad and onto clothes)
5. Anaemia (low iron count in the blood)
What are the causes of heavy menstrual bleeding?
Dysfunctional uterine bleeding
When we cannot find a physical abnormality to account for the heavy menstrual bleeding, we say it is ?dysfunctional uterine bleeding?. In a way this means we do not know exactly what the problem is but it is probably due to very subtle hormone changes. These hormone changes are so small they do not come up on the normal blood tests we do for hormones.
Fibroids
Fibroids are non-cancerous growth inside the uterus which can cause heavy menstrual bleeding. Please have a look in the section ?fibroids? for further information.
Polyps
Polyps are non cancerous little growths which arise from the lining of the uterus. They are more likely to cause bleeding outside the normal periods, rather than heavy menstrual bleeding.
Cancer of the uterus, cervix or vagina
Your doctor will always make sure that there is no cancer to account for the heavy bleeding. The gynaecological examination and ultrasound of the uterus can give an indication as to the likelihood of something more serious going on. These are one of the more uncommon causes of heavy menstrual bleeding and are more likely to cause bleeding after menopause, bleeding between periods or a blood stained vaginal discharge.
Will I need some tests for my heavy or irregular periods?
It is important to find out why your periods are heavy or irregular. Your doctor will order an vaginal ultrasound to check the lining of the uterus. Instead or after the ultrasound you may need a hysteroscopy and curettage. Please have a look under the section "hysteroscopy" for further information. A hysteroscopy is a day procedure where your doctor inserts a telescope like instrument from between the legs into the vagina and uterus. The inside of the uterus is then visualized and any abnormalities seen. Curettage means samples (biopsies) are taken from the lining of the uterus, so the pathologist can have a look at them through a special microscope and see if there are any abnormal cells.
What are my choices for making my periods lighter?
If the ultrasound or hysteroscopy showed up an abnormality like a polyp or fibroid that your surgeon removed, you may wait and see if that made a difference to your periods.
There are medical and surgical treatment options for heavy menstrual bleeding.
Medical treatment options
Non steroidal anti-inflammatory medications (NSAIDs)
NSAIDs are medication like aspirin, naproxen (i.e.. Naprogesic, Naprosyn), ibuprofen (i.e. Brufen, Nurufen) etc. These tablets reduce menstrual flow by about one third and are also good for period pain. They should be taken with food and side effects are stomach upset, nausea and diarrhoea.
Oral contraceptive pill
The oral contraceptive pill (OCP) reduces menstrual bleeding by about one third as well and can also reduce period pain. The more common side effects of the pill are nausea, breast tenderness and headaches. Women who are over 35 years old and smoke should not take the pill because of the risk of deep vein thrombosis (clots in the leg veins).
Progesterone
Progesterone medications cause thinning of the lining of the uterus. It can be taken for three weeks every month as a tablet from days 5 to 25 of the menstrual cycle (day 1 is first day of periods). Side effects are breast tenderness, bloating, weight gain and weight gain.
Tranexamic acid
This tablet reduces menstrual bleeding by about 50%. It works by acting on the clotting mechanism of the lining of the uterus. Diarrhoea and are uncommon side effects. It is taken four times a day only for the first four days of periods.
Mirena intrauterine device
The Mirena intrauterine device (IUD) is a small device, the size of a 50 cents piece, which is inserted into the uterine cavity. It is the most effective treatment modality out of all the above options and has one of the least side effect profiles.
It contains a hormone called progesterone which is a hormone that the ovaries naturally produce in the body. This hormone is slowly released into the uterus and causes the lining to become very thin. Hence periods become either very light or there is no bleeding at all. The Mirena can stay for five years and may be removed at any time before that if the woman wishes so.
A woman needs to know the following before she agrees to the Mirena :
There will be irregular vaginal bleeding for the first 3-6 months because that is the existing lining of the uterus coming away. Once the lining has become thin, this irregular bleeding stops and she will experience either light periods or no periods at all.
The Mirena is one of the most efficacious contraceptives. However, like all contraceptives, it has a failure rate. Two in 1000 women who has the Mirena will get pregnant. Severe infection, miscarriage, premature delivery or death of the baby may occur if a woman becomes pregnant with the IUD. Therefore it is recommended that the Mirena is removed which may cause a miscarriage.
There are side effects of the Mirena. Please have a look at the Mirena website at www.mirena-us.com for further information. Your doctor will discuss the possible side effects with you prior to its insertion.
Surgical treatment options of heavy menstrual bleeding
Endometrial ablation
At endometrial ablation the lining of the uterus is burnt with an instrument that is placed inside the uterine cavity. It is done as a day procedure with a light anaesthetic (medication through the vein for sedation and local anaesthetic in cervix).
Hysterectomy
Hysterectomy refers to the surgical removal of the uterus. Please have a look in the section "hysterectomy" for further information.
Back to Top
ABNORMAL PAP SMEARS
What is a Pap smear?
A Pap smear is a screening test to see if abnormal changes are present in the cervix of the uterus. The cervix is the lowest part of the uterus which can be seen at the top of the vagina.
Your doctor inserts a speculum into the vagina so that the cervix can be visualized and a scraping of the cells from the cervix is taken with a little brush. The scrapings are then prepared on a microscope glass slide and also placed into a vial of preparation fluid (Thin Prep). These are then sent to a pathologist who looks at the specimens under a microscope.
If the cells are abnormal, your GP or gynaecologist will explain the result to you. Dr Varol will also give you a pamphlet for your reading. Abnormal cells are precancerous and some abnormalities may need treatment to be removed, so cervical cancer does not develop.
Every women should have a routine Pap smear every two years, so precancerous abnormalities can be detected early and treated, if necessary. Precancerous abnormalities usually do not cause any pain or other physical symptoms, so a Pap smear by your doctor is the only way to find out whether everything is ok or not.
What does the abnormality on my Pap smear mean?
The important abnormality of the cells is called dysplasia which is not cancer, but can develop into cancer over a long but unpredictable period of time. Abnormalities on Pap smear are graded and classified as low or high grade. The precancerous changes involve only cells in the surface layer of the cervix.
Low & High Grade Abnormalities
Pap smear results are reported as low or high grade abnormalities, CIN (cervical intraepithelial neoplasia) or dysplasia. Intraepithelial means ?within the tissue? and neoplasia ?new growth of abnormal cells?. They all describe changes of the cervix which may develop into cancer. The more severe the abnormality, the less likely it is to go away and the more likely it is to get worse and become cancer. So treatment is necessary for the more severe abnormalities to prevent cancer of the cervix from happening. The table below shows these terms.
Dysplasia | Cervical intraepithelial Neoplasia (CIN) | High/Low grade abnormality |
Mild dysplasia | CIN 1 | low grade abnormality |
Moderate dysplasia | CIN 2 | high grade abnormality |
Severe dysplasia | CIN 3 | high grade abnormality |
Atypia & Non-specific Minor Changes
These minor changes seen in a Pap smear are usually due to tissue inflammation, the human papilloma virus, or other infections such as bacteria, yeast (?thrush?) etc. Usually this Pap smear goes back to normal by itself and needs to be repeated in 12 months. It is very important that you come back for your Pap smear in 12 months.
If the abnormality persists, you will advised to have an examination called colposcopy see under heading ?colposcopy?
Cervical Intraepithelial Neoplasia (CIN 1)
CIN 1 falls into the low grade abnormality category, whilst CIN 2 and 3 into the high grade group. In about 60% of women with CIN 1 this abnormality will disappear by itself. In the remaining 40%, CIN 1 will persist or become a higher grade. Your doctor will advise you whether you just need another Pap smear in 6 months to see if the abnormality has gone, or you may need to have a colposcopy and biopsy by your gynaecologist.
High-Grade Abnormalities
CIN 2 and 3
CIN 2 and 3 mean that the precancerous abnormalities are high grade. These abnormalities require treatment to remove the abnormal cells. Depending on your doctor"s examination findings with the microscope (colposcopy) and the biopsy of the cervix, some women with CIN 2 may have the conservative option to repeat all the investigations again in four to six months.
What is going to happen at the gynaecologist?
Colposcopy
If a minor abnormality persists with repeat Pap smears or if a high grade abnormality is present, an examination called colposcopy is needed. The gynaecologist will insert a speculum into the vagina so the cervix can be seen. He/she then looks at the cervix with a colposcope which is a magnifying instrument similar to pair of binoculars on a stand and a light attached. The colposcope itself does not enter the vagina. The cervix is then painted with a solution called acetic acid (dilute vinegar) and the doctor looks for abnormal cells.
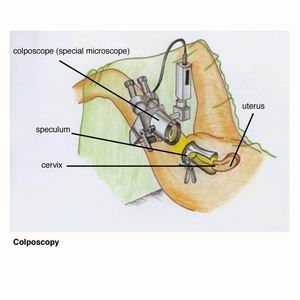
This examination takes 10-15 minutes and is not a painful procedure. Some women experience discomfort from having the speculum in the vagina.
Biopsy
Your doctor may need to take a very small sample of tissue from the abnormal part of the cervix. This is called a biopsy. A special solution is then applied to the biopsy site to stop bleeding. You may experience some pain or discomfort similar to menstrual cramping. After the biopsy you may have slight vaginal bleeding and a vaginal discharge for up to a week. Avoid vaginal intercourse, tampons, swimming and baths (shower instead) for a week to allow the cervix to heal.
What causes abnormalities on Pap smear?
The precancerous abnormalities are caused by the Human Papilloma Virus (HPV), also called wart virus, and cigarette smoking. HPV is similar to the virus which causes warts on other parts of the body, such as the hands and feet. HPV is part of being sexually active and most men and women who are sexually active, do have HPV. In the vast majority of people, HPV infection is transient and harmless and the body"s immune system clears it within about two years.
So if the Pap smear just shows HPV only, then no further treatment is necessary. However, in some women persistent infection with some types of HPV causes precancerous abnormalities on the cervix. The doctor would then recommend a colposcopy and biopsy.
The tobacco in cigarettes has been shown to cause precancerous abnormalities on the cervix and cervical cancer. So if a woman smokes and has an abnormal Pap smear, she should very seriously consider stopping smoking.
Will I need further treatment?
If the results of the colposcopy and cervical biopsy show a high grade abnormality, treatment is required to remove the abnormal cells. There are several methods to remove the abnormal area of the cervix which depends on the type and severity of the abnormal cells and the gynaecologist"s preference.
Wire Loop Excision
In this method, the abnormal cells are scooped from the cervix with a wire loop.
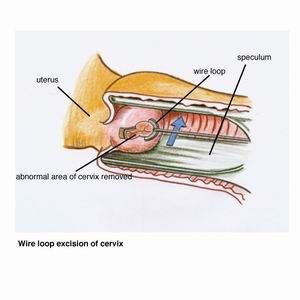
A local anaesthetic is needed and the procedure takes 15 to 30 minutes and is performed in a day procedure centre, doctor"s surgery or hospital outpatient department. A bloody brown, or black discharge will be present for up to four weeks after the procedure. Some mild tummy cramps or pain may persist for a day or two afterwards as well. Most women can return to work within two or three days after the procedure.
The abnormal part of the cervix that has been removed is then sent to the pathologist
who :
- confirms whether all the abnormal cells have been removed, and
- determine the type of abnormality present.
Laser
The abnormal cells are destroyed using heat from a laser beam which is an intense, highly focused beam of special light). Again this procedure is performed in a day procedure centre, doctor"s surgery or hospital outpatient department.
Cone biopsy
For a cone biopsy a cone-shaped section of the cervix containing the abnormal cells is removed.
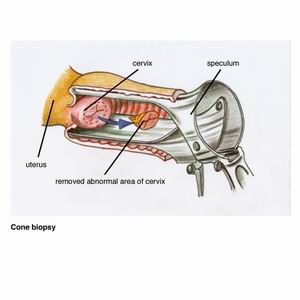
This usually requires a general anaesthetic and a day hospital stay. A cone biopsy is donewhen :
- Pap smear showed abnormal changes in the glands of the cervix
- abnormal cells go up in the cervical canal
- to exclude cervical cancer.
Will treatment affect my chances of becoming pregnant?
No, treatment does not cause infertility. However, there is a slightly increased risk of cervical incompetence with a cone biopsy and loop excision. Cervical incompetence means that the cervix does not stay closed during pregnancy and can open up, resulting in a miscarriage in the mid trimester of pregnancy, that is, between about 3 to 6 months of pregnancy. If it is recognized in time, the obstetrician would place a stitch into the cervix under a general anaesthetic in the operating theatre. The stitch is removed when it is time to deliver the baby.
Another complication can occur called cervical stenosis. This means scar tissue has formed in the cervix and it has become closed off. Menstrual fluid cannot flow into the vagina and tummy pain may occur. The gynaecologist would need to dilate the cervix in the operating theatre under a light anaesthetic.
What are the potential complications of treatment?
Following treatment to remove the abnormal cells of the cervix, bleeding and infection may occur. This may require antibiotics through a drip in the arm and admission in hospital. For the bleeding the doctor may place a tissue pack into the vagina to keep pressure on the cervix for about 24 hours. Alternatively a suture may be needed in the cervix in the operating theatre.
Cervical incompetence and stenosis have been explained above.
What follow-up do I need to have?
Follow-up depends on the abnormality and your doctor will formulate a plan with you. You may need to come back in six or 12 months for a low grade abnormality. Following treatment for a high grade abnormality, follow-up is usually at four to six monthly intervals initially, then yearly until two consecutive Pap smears, colposcopy and HPV tests are negative (normal).
Back to Top
Obstetrics
Our female-only practice now offers comprehensive obstetrics care that is highly individualised. Our obstetricians Dr Joyce Wu and Dr Gemma Blain have extensive experience in managing both high risk and low risk pregnancies, and are dedicated to providing you with the best evidence-based advice and practice in caring for your pregnancy.
At your first consultation, your personal and medical history will be explored and discussed with its potential implications in pregnancy. You will also be informed of the schedules of all the antenatal appointments, recommended scans, blood tests, and vaccinations. Delivery plans will be revisited throughout out pregnancy so you can make an informed decision that best suits the needs of you and your family. We will also assist with your decision on the hospital you wish to deliver at, depending on your geographic location, personal needs, and risks in pregnancy after assessment.
At each appointment any new blood or scan results will be reviewed by our obstetricians with a plan for further tests if required. In addition to routinely assessing your blood pressure and abdomen, your baby will be visualised through our bedside ultrasound at each visit. If any concern arises from the antenatal assessments, you will be notified and referred for additional investigations.
Both being mothers of young children, Joyce and Gemma understand the stress that women frequently experience in pregnancy. We also understand that complications can arise unexpectedly that can heighten the anxiety in pregnancy. Joyce and Gemma are equipped with the knowledge and skills that manage your pregnancy, whether it is low risk or complicated. We offer psychological support by sharing experiences, and referring for appropriate professional counselling services when indicated. By limiting the number of pregnant women we care for, we are able to dedicate our time and effort to each woman throughout pregnancy and delivery.
We believe our comprehensive and professional pregnancy service will provide our women a very unique and pleasant experience in this special period of life. Please contact our friendly reception staff and we will be happy to assist with your enquiries.
The Hospitals Dr Gemma Blain deliver at:
Royal Prince Alfred Hospital
The Mater Hospital
North Shore Private Hospital
The hospitals Dr Joyce Wu deliver at:
Royal Prince Alfred Hospital
The Mater Hospital
North Shore Private Hospital
Northern Beaches Hospital (from Nov 2018)
Dr Joyce Wu also consults in Mandarin.