Your Health This information package is designed for general information and is not a substitute for a medical opinion. It will help you to make an informed decision after you have discussed your options with your doctor and a tailor-made care plan has been formulated.     What is endometriosis? The uterus (womb) has a cavity in which a baby grows. Part of this lining (called endometrium) is shed every month and results in menstruation (a period). When this lining grows outside the uterus, we call it endometriosis. One in ten women (10%) of menstruating age have endometriosis, so it is considered common. It can occur from the age of puberty to beyond the menopause as well.   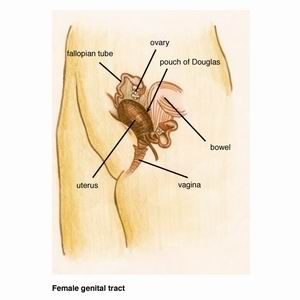       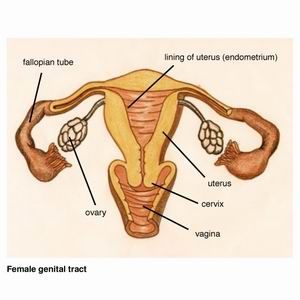 Endometriosis causes scar tissue and can result in the uterus, ovaries, fallopian tubes and bowel becoming stuck to each other and to the lining of the tummy. Here are some photos of what endometriosis looks like and photos of endometriosis that has been excised (cut out) for treatment.   
  What causes endometriosis? Although the exact cause of endometriosis is still unknown, there are a number of theories about how it develops. It is believed that a number of causes exist together to cause this disease. The most likely explanation is that cells lining the tummy change into the type of cell that line the uterus. Some endometriosis probably results from menstrual fluid flowing backwards through the fallopian tubes and deposits in the tummy. There is a genetic component to endometriosis and women who have a mother or sister with endometriosis, are more likely to have it as well. There is a change in the immune system in women with endometriosis. Most women have a natural defense which gets rid of menstrual fluid in the tummy. Women with endometriosis have a reduced ability to clear it or to prevent its growth once it has settled on the lining of the tummy. The hormone oestrogen produced by the ovaries is also required to grow endometriosis. That is why after the menopause when the ovaries stop functioning and the oestrogen becomes very low, usually the pain with endometriosis settles down.   Factors reducing the risk of endometriosis 1. Aerobic exercise of five hours per week has been shown to reduce the risk of recurrence of endometriosis. 2. Having a child reduces the risk of recurrence by about 50%. 3. Similar to pregnancy, the oral contraceptive pill also has a protective effect. It keeps the ovaries quiet and there is no ovulation (egg production and release). The pill prevents the surge in oestrogen that normally occurs.     What problems does endometriosis cause?   Pain with periods This is the most common pain with endometriosis. Period pain usually starts with the first time a woman has her periods. In many women period pain may start after many years of having fairly pain-free periods. These women particularly are likely to have endometriosis. However one needs to remember that about 70% of women in the world have period pain that is normal without any underlying reason except that they are having periods. A woman may not have any pain despite quite advanced endometriosis. She may see her doctor because she cannot get pregnant. The severity of endometriosis often does not correlate with the severity of pain. Women with little endometriosis may have a lot of pain or they may have a great deal of endometriosis and not much pain at all.   Pain with sex If there is endometriosis on the vagina and forms scar tissue, it can be painful during sex because the vagina cannot stretch. Pain may also occur due to nerves being involved in that area. Pain can particularly be painful when vaginal intercourse occurs just prior to periods (or during periods if vaginal intercourse occurs during that time).  
  Pain when opening bowels Pain that occurs when a woman opens her bowels is usually an indication of advanced endometriosis. Endometriosis would involve the wall of the bowel or may just cover the space between the uterus, vagina and bowel. This area is called the pouch of Douglas and basically is the area a woman sits on, that is, the bottom of the tummy. Here is a diagram and a photo of this area. 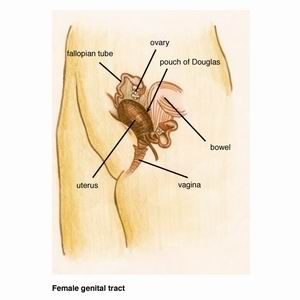  
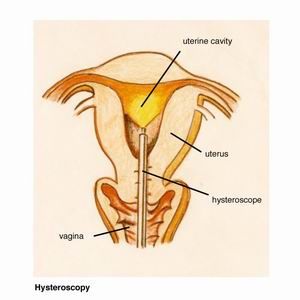
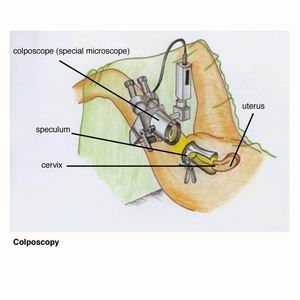
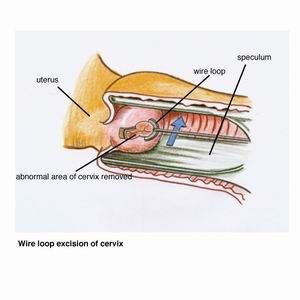
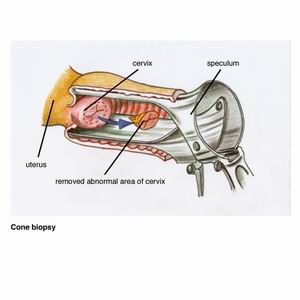
Pain when opening bowels can sometimes be so severe that a woman is doubled over in pain on the bathroom floor.   Examination A gynaecological examination by your doctor is very important. Your GP or gynaecologist would have a feel of your tummy, and then examine the vagina with a speculum. This is the instrument used to take a Pap smear. A vaginal examination is then performed which may reveal an area of tenderness. The doctor may also feel some nodularity in the vagina which would indicate scar tissue behind the vagina or on the bowel.   Often the gynaecological examination is perfectly normal. This does not exclude endometriosis, as a woman may still have mild or moderate disease which has not caused significant scar tissue to be able to be felt on vaginal examination.   Ultrasound The only abnormality an ultrasound would pick up is a cyst of endometriosis in the ovaries. This is called a ?chocolate cyst? because it is filled with old blood that looks like melted chocolate.  When we see chocolate cysts in the ovaries, it usually means advanced endometriosis. In general these cysts develop once endometriosis has grown in a lot of areas of the tummy already.   Laparoscopy Laparoscopy is the only way we can make a definite diagnosis of endometriosis. This is also called ?keyhole surgery? which is done under general anaesthetic in hospital. Very small cuts (half a centimeter) are made in the tummy and a laparoscope (this is like a telescope) is inserted through the belly button. The laparoscope is connected to a camera and television, so the surgeon can visualize all the gynaecological organs. 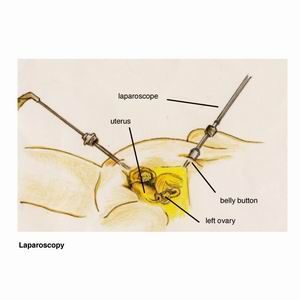     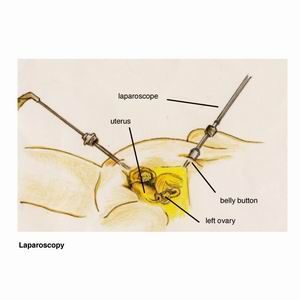 Here are photos of what a normal pelvis and abdomen look like.
If endometriosis is present, the surgeon excises it (cuts it out). Laparoscopic excision of endometriosis requires a high degree of skill by the surgeon. Therefore the surgeon would have had special training in this type of operation.   Laparoscopy has many advantages over open surgery where a big cut is made in the tummy, like a caesarean section cut. Women experience much less pain, recover more quickly, there is minimal scarring and reduced risk of infection   Please have a look under the heading ?Laparoscopy?   Peritoneum The peritoneum is the lining of the pelvic organs. Endometriosis most commonly affects the peritoneum.
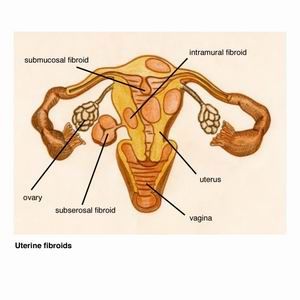
  Ovary A cyst of endometriosis in the ovary is called a ?chocolate cyst? because it is filled with old blood that looks like melted chocolate. The medical word for it is endometrioma. Here is an example of an endometrioma.  
Uterus Endometriosis is often seen on the back of the uterus where it affects the outer layer. One can see reddish or clear coloured areas of endometriosis. Here is an example of endometriosis affecting the uterus.
Complete obliteration of pouch of Douglas. The bowel is densely adherent to uterus, so only top of uterus is visible. No normal anatomy of pouch of Douglas is present. Rectum and vagina When endometriosis affects the vagina, women often feel pain during sex. This occurs because scar tissue prevents the vagina from stretching or because nerves are affected by endometriosis. The rectum is the lowest part of the bowel behind the anus. The anus is where one opens the bowels. When endometriosis affects the bowel, women have pain with sex and on opening bowels. Rarely bleeding from the anus may occur during periods. Here is an example of endometriosis affecting the rectum and vagina.  
  Bladder Endometriosis often affects the lining over the bladder. Rarely it can go deeper into the muscle of the bladder and cause pain when a women passes urine or there may be blood in the urine. Here is an example of endometriosis affecting the lining over the bladder.  
  Below ribcage or diaphragm Rarely a women may have endometriosis in the lining underneath the ribs higher up in the tummy. This can cause pain in the upper tummy during periods. Here is an example of endometriosis below the ribcage on the right.  
  Endometriosis and infertility! Endometriosis is commonly associated with infertility. About 30% of women requiring IVF infertility treatment (in vitro fertilization or ?test tube babies?) have endometriosis. It is important to find out about endometriosis early , so it can be treated and infertility isprevented or minimized.   Here are some of the previous photos which explain why a woman would not be able to become pregnant. When the anatomy is distorted, the tubes become blocked, the egg does not get picked up by the tube and cannot travel through the tube to implant inside the uterus.
  Other diseases may be confused with endometriosis Many women have irritable bowel disease with pain in the tummy, bloating, constipation and diarrhoea. The pain may be similar to endometriosis pain. Whilst pain gets better in the majority of women after endometriosis surgery, sometimes scar tissue may form in the tummy which can cause pain that can be similar to the pain of endometriosis.   What endometriosis is NOT associated with Endometriosis does not cause heavy or irregular periods. If a woman has lots of bleeding with her periods, the doctor will help her with that separately. The only menstrual irregularity endometriosis can cause is some spot bleeding a few days before the proper periods start.   What about drug treatment? The best drugs for period pain are tablets which are called non steroidal anti inflammatory drugs. These are like aspirin such as Ponstan, Nurufen, Naprogesic etc. They give better relief from period pain than paracetamol (Panadol).   Because not all period pain is from endometriosis, some women decide to try the oral contraceptive pill. The pill acts by preventing ovulation (release of egg from the ovary) and stopping the large oestrogen surge from the ovary. The pill is usually given continuously by skipping the sugar tablets, so that there are no periods. This often causes breakthrough bleeding where bleeding occurs at any time when the pill is taken. So realistically a woman needs to have a proper period on the pill every 3 to 4 months to stop that annoying bleeding.   A woman may decide to take the pill for pain control rather than opt for a laparoscopy because a laparoscopy is an operation with associated risks and she does not want to go down that path.  Studies have shown that after laparoscopic surgery for endometriosis, the disease may come back in about 30% of women. To minimize the recurrence of endometriosis, it is advised to commence hormonal treatment after surgery. The Mirena intrauterine device is often the best way to do that. It is highly effective in reducing the bleeding from periods or may even stop monthly periods and has very little side effects. Alternatively the pill may be given. For women who had severe endometriosis at surgery, she may be treated with a stronger drug called Zoladex for six months before switching to the pill or continuing with the Mirena. |

|